Medical Insurance a Revenue Cycle Approach Chapter 2 Review Questions Answers Quizlet
The Impact of Healthcare Regulations
With recent authorities regulations affecting the healthcare industry, healthcare practices have been impacted in numerous ways. Sure third-party wellness insurance payers have negotiated fee-for-service contracts with providers, which has resulted in lower reimbursement. HIPAA, the Healthcare Insurance Portability and Accountability Human action has also had an touch, by tightening the requirements for claim data submission. And equally the healthcare organization transitions from a fee-for-service a value-based reimbursement model, healthcare practices and providers have had to arrange the way they bill for care provided. Due to these changes in government regulations, having a good for you revenue wheel is more important than ever.
What is a Revenue Bicycle?
What exactly does the term "acquirement cycle" mean? The revenue cycle is defined every bit all authoritative and clinical functions that contribute to the capture, direction, and collection of patient service revenue. In the most simplistic and basic terms, this is the entire life of a patient account from creation to payment.
A healthy revenue cycle should follow billing and collection best practices to ensure bills are submitted in accord with payor requirements and all services provided are billed. The last affair that a healthcare organization needs is to provide services and non be paid.
Revenue Cycle Leakage Points
In that location are many different leakage points in the revenue cycle, but hither are the most common:
- No referral
- Registration, coding or billing errors
- Unverified insurance
- Underpaid claims
- Denied appeals

Professional Billing & Collection Best Practices
At that place are various all-time practices your healthcare organization can incorporate for a healthy revenue cycle. By using data to compare to these "standards", organizations have the ability to understand leakage points and opportunities for improvement. Some of the best practices include:
- Carry Financial Clearance – This includes maintaining and verifying patient information before the patient arrives for their date. Insurance eligibility is checked and authorizations are tracked. Patients are notified of outstanding balances and prompt payment is encouraged.
- Streamlined Check-In & Check-Out Process – Patient information is confirmed and verified, eligibility determination is conducted; prior and new balances are collected.
- Accuse Capture – An electronic charge capture process is utilized; specific coding situations are managed; documentation audits are performed.
- Charge Entry – During this stage, fee schedules are developed and managed; charges are entered; charges are reviewed and audited; the person responsible for editing charges is strictly controlled.
- Proper Claims Management – Electronic claims are submitted and status updates are frequent; secondary merits procedure happens; attention is paid to maintain compliance with insurance carrier's claim format requirements; at that place are multi-tiered claim editing checks; assistance with edit tracking and error resolution happens; a system for piece of cake rebilling or corrected claim processing is implemented; and an overall analysis of billing procedure delay times is taking identify.
- Patient Statements – In the patient statements stage, cycled billing occurs; statements are clear and curtailed; in that location are notes and automated holds on patient statements when applicative; final notices get out.
- Payment & Deprival Posting – This phase includes the entering of payments; the managing of contractual write-offs; the processing of insurance reversals; credit residue resolution; the review of denials and adjustments; and the control of who tin edit payments.
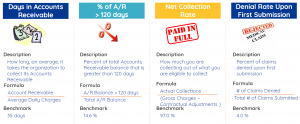
- Insurance Follow Up – Verification that insurance carriers are receiving claims and that the claims are being processed; accounts receivable are worked on by priority; staff's collection actions are audited; your practice's average days in accounts receivable and net collection rates are known.
- Denial Direction – During deprival direction, you'll know if your claims denials charge per unit is excessive; at that place is understanding of the claims denials received; your common denial causes are analyzed to meliorate processes; and denied claims are resubmitted if payment can notwithstanding be collected.
- Patient Collections – During the patient collections stage, patient billing occurs; collection letters are sent; general collections take identify; payment plans are offered; patient balances are reviewed earlier appointments; the productivity of collectors is analyzed.
- Payor Direction – In this stage, attention is paid to fee schedules, carrier provider numbers and NPI, assignment of benefits, carrier communications and contract dates, documentation to support claims, and carrier analysis take place.
Mutual Revenue Bicycle Best Practice Metrics
All Thought Leadership
We use cookies to ensure that we requite you the best possible experience on our website.Take Reject Read More
Source: https://afiahealth.com/understanding-the-healthcare-practice-revenue-cycle/
0 Response to "Medical Insurance a Revenue Cycle Approach Chapter 2 Review Questions Answers Quizlet"
Post a Comment